Anxiety stress in brain, overload in mind. Depression, adhd, ocd.
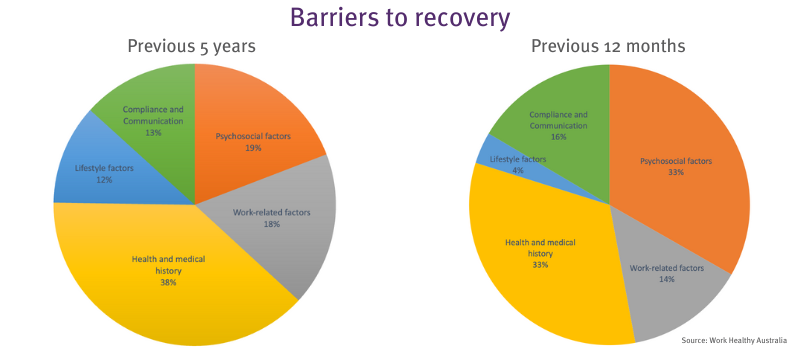
Psychosocial factors are increasingly identified by insurers as barriers to recovery for injured workers – often leading to longer claim duration, higher costs and poorer long-term outcomes if not addressed in the early stages.
33 per cent of patients seen by a Work Healthy Australia clinician in the last 12 months have cited psychosocial factors as a barrier to their recovery. This has increased by 15 per cent in the past five years, which may be attributed to such factors as the COVID-19 pandemic, labour shortages causing pressure in the workplace, and the increasing cost of living.
According to Safe Work Australia, a psychosocial hazard is anything that could cause psychological harm (e.g. harm someone’s mental health). Common psychosocial hazards at work include:
- job demands
- low job control
- poor support
- lack of role clarity
- poor organisational change management
- inadequate reward and recognition
- poor organisational justice
- traumatic events or material
- remote or isolated work
- poor physical environment
- violence and aggression
- bullying
- harassment, including sexual harassment, and
- conflict or poor workplace relationships and interactions
It’s important to look at the bigger picture
Every worker’s journey, even for the exact same injury, poses unique challenges when it comes to re-engaging an individual back to their job. Adopting a biopsychosocial approach (looking at the bigger picture) to managing musculoskeletal injuries helps acknowledge the individual experience of pain and navigate underlying psychosocial barriers that may be present.
Pain can be complicated by seemingly unrelated stresses such as financial pressures, cultural and gender norms, previous advice from medical professionals and, our favourite, “Dr Google”. The literature regarding pain tells us that no two people process the pain experience the same way, and that the severity of pain does not equal the severity of injury.
Identifying psychosocial barriers to recovery
The following are some potential signs that psychosocial barriers to recovery exist:
- High pain catastrophising: e.g. a worker reporting high levels of pain that are inconsistent with their injury or their behaviour
- Dependence of passive treatment: e.g. worker demanding weekly treatment sessions with the onsite health provider
- Disgruntled feelings: e.g. worker is dissatisfied with the workplace support or how they were injured
- Negative expectations: e.g. worker believes they won’t get better or that they will have this pain/injury forever
- Over-identification with injury/diagnosis: e.g. worker will be overly concerned about the way the injury occurred or the way the injury affects their body
What can we do?
Early intervention is best practice
Workers who engage with practitioners in an early timeframe are more likely to have psychosocial factors identified early, enabling a ‘person-centred’ approach to address these barriers with a graduated return to work.
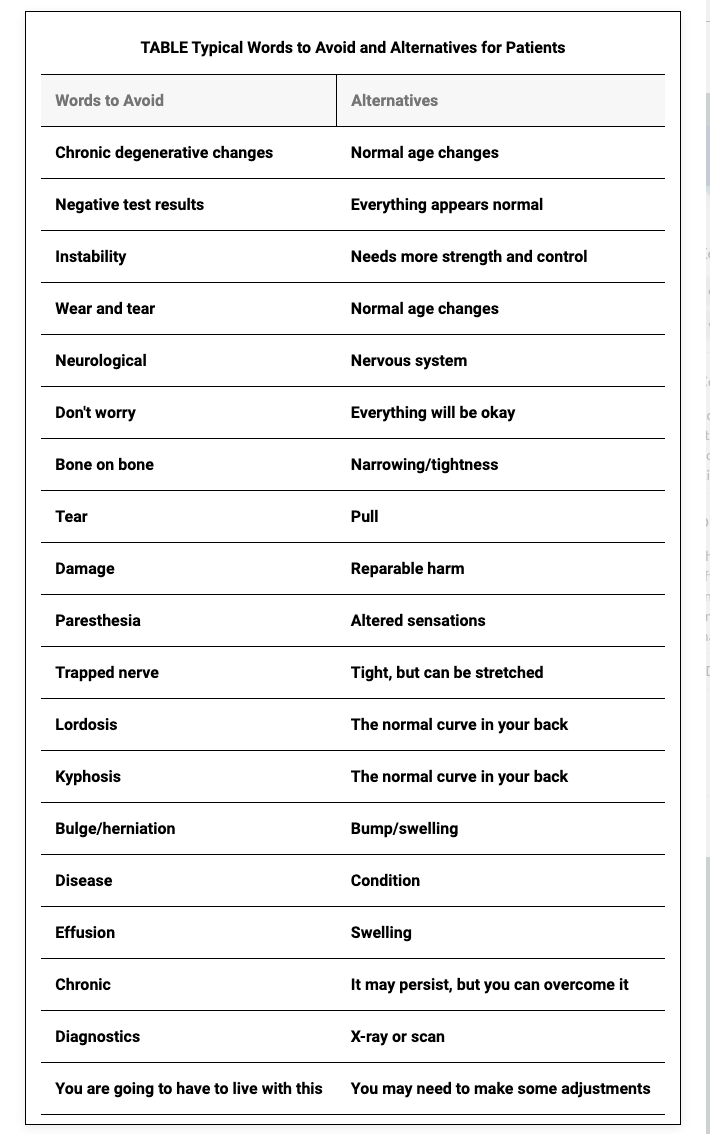
Adopt “words that heal”
At Work Healthy Australia, our providers are trained to engage with a biopsychosocial approach to pain. This means that we appreciate that pain is not just one dimensional and is often nuanced by our past experiences and a worker’s health literacy.
One simple takeaway your team can use going forward is to address the language we use with regards to common medicalised terms.
An important delineation is that we do NOT downplay people’s pain. Our experience of pain is true to us and that must be preserved. However, we can ensure that our words are not inflammatory to people’s experience of pain or set poor expectations for recovery from the painful experience.
Legislative requirements
In April 2023, new Commonwealth work health and safety laws (Work Health and Safety Regulations 2011) came into place, prescribing how employers must identify and manage hazards and risks to workers’ psychological health and safety. For information on these changes, refer to Safe Work Australia, Comcare and your state Workcover authority.
Sign up to our monthly enewsletter
"*" indicates required fields
