People, healthcare and problem concept - unhappy man suffering from neck or shoulder pain at home
Pain is a common experience that affects various aspects of our lives, including the workplace. It is also complex, and very individual. Understanding pain better can help you to support those around you who are experiencing it.
We spend a significant portion of our time at work, so it is crucial to recognise and address the impact of pain on workers’ wellbeing, productivity, and overall job satisfaction.
3.37 million Australians were living with chronic pain in 2020, and of those, 68.3% are of working age.
What is pain?
According to Pain Australia, pain is an unpleasant feeling, causing a reaction to protect the part that is painful. If you have experienced pain before, you know what it is, but that doesn’t mean you understand another person’s pain. Pain is a subjective experience. To make it even more complex, different factors affect how we experience pain. Our emotions, our social support system, our past history, our genetics and our environment influence our perception of pain.
What causes pain?
Pain can be related to a particular health condition, accident or injury (e.g. falling down the stairs and hurting your knee), have a gradual onset (e.g. due to repetitive movements and overuse), or have no clear cause or reason.
Pain becomes chronic when it goes on for more than three months, or past normal healing time. Common conditions related to chronic pain include:
- Low back pain
- Neck pain
- Arthritis
- Headaches and migraines
- Fibromyalgia
- Cancer
- Endometriosis
- Neuropathic (nerve pain)
Chronic pain can affect a person’s ability to perform job duties effectively. The physical and psychological toll of chronic pain can lead to absenteeism, presenteeism (being at work but not fully engaged or productive), and decreased job satisfaction.
Best practice pain research recommends a whole-person view and a multidisciplinary approach.
“To be successful pain managers, we may have to use a combination of strategies such as medications, movement, diet, relaxation, thinking strategies, and more.” (Chronic Pain Australia)
The bio-psychosocial model of pain
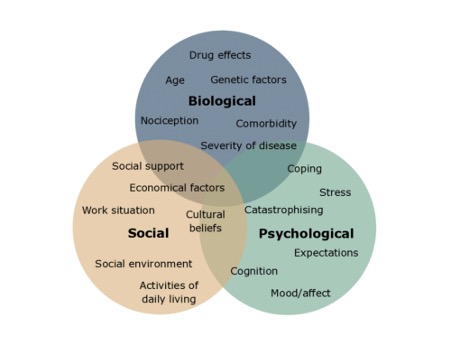
As we noted before, pain is a complex subjective experience that is affected by many factors. The bio-psychosocial model of pain describes the dynamic interplay between biological, psychological, and social factors that vary from individual to individual. Understanding this and exploring the topic of empathy is critical for supervisors and managers to assist in their workers’ and team’s recovery.
Treating everyone as an individual
“We need to treat everyone as an individual”, says Cameron Hooper, Workplace Health Provider at Work Healthy Australia. “Everyone is on their own journey which includes periods in our lives when we experience pain.”
“You have to listen to each patient and try your best to understand their story. You have to treat them as if they were your mother, your sister or brother. Treat them with that level of respect and care. You are there to see the person in front of you. Respect them and do your best to help them,” he says.
Barriers to admitting pain in the workplace
Cameron says that in his experience, some workers are fearful of losing their job or income if they seek treatment for a sore joint or an injury. Some injured workers might be having troubles at home, financial stress, going through conflict at work, or worrying about their children. All these things can impact their pain and are important for us to appreciate.
Cameron, says that as he treats his patients for musculoskeletal injuries, he listens to their stories, learns about their backgrounds, their workplace dynamics.
“This forms an important part of the treatment,” he says. “I’ve treated workers who were experiencing pain but didn’t feel their supervisors or managers believed them. Having unsupportive managers and not being believed can add negatively to their pain experience and recovery process.”
Our headspace is crucial for faster recovery and better prognosis. If the patient feels they are not being heard, not being believed, their supervisor is not demonstrating empathy or understanding, it creates a cycle that will negatively impact that their recovery. We need to cultivate an optimum environment for workers.
What can you do to support your employees?
- Create a culture of empathy, understanding, and support where employees feel safe and comfortable discussing their pain-related challenges without fear of stigma or negative consequences.
- Offer flexible work arrangements such as adjustable working hours, remote work options, or modified duties to accommodate the needs of employees experiencing pain. This allows them to manage their pain more effectively while maintaining productivity and engagement.
- Encourage open lines of communication between employees and their managers or HR departments to discuss pain-related challenges. Provide reasonable accommodations, such as ergonomic adjustments, assistive devices, or modified job tasks, to help employees manage their pain and continue performing their duties effectively.
- Promote the availability of EAP services that offer confidential counselling and support for employees with chronic pain. EAPs can assist employees in coping with the emotional and psychological aspects of pain.
- Conduct training sessions in collaboration with your onsite health provider to educate employees, supervisors, and managers about chronic pain conditions, the bio-psychosocial model of pain management, and strategies for supporting employees experiencing pain. This can foster a better understanding and empathy within the organisation.
- Regularly communicate with your onsite health provider and other health professionals your employees might access (such as GP, and pain management specialists)
- Develop personalised return-to-work plans in collaboration with your health providers and employees to ensure a smooth transition back to work after a period of absence due to pain. These plans should consider individual needs, accommodations, and a gradual increase in work responsibilities.
By implementing these strategies, you can create a supportive environment that helps employees with pain effectively manage their condition, maintain productivity, and improve overall wellbeing.
Further resources
Sign up to our monthly enewsletter
"*" indicates required fields